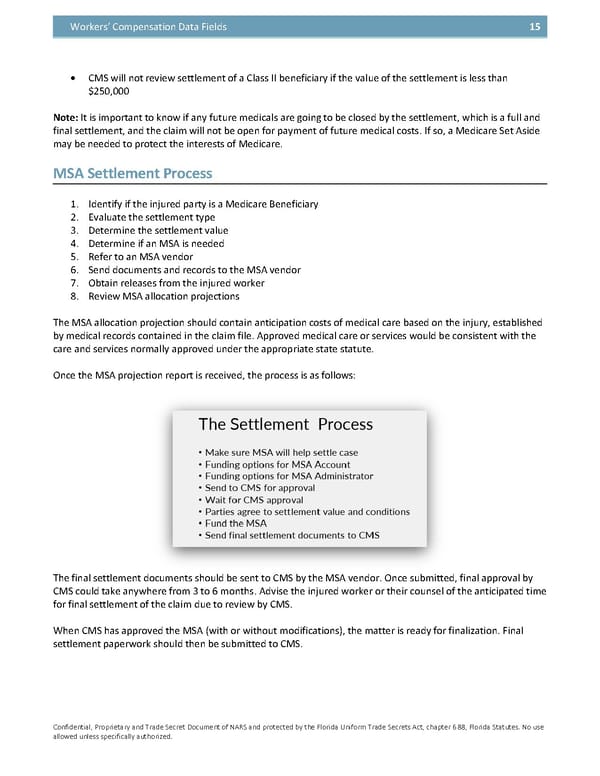
Workers’ Compensation Data Fields 15 • CMS will not review settlement of a Class II beneficiary if the value of the settlement is less than $250,000 Note: It is important to know if any future medicals are going to be closed by the settlement, which is a full and final settlement, and the claim will not be open for payment of future medical costs. If so, a Medicare Set Aside may be needed to protect the interests of Medicare. MSA Settlement Process 1. Identify if the injured party is a Medicare Beneficiary 2. Evaluate the settlement type 3. Determine the settlement value 4. Determine if an MSA is needed 5. Refer to an MSA vendor 6. Send documents and records to the MSA vendor 7. Obtain releases from the injured worker 8. Review MSA allocation projections The MSA allocation projection should contain anticipation costs of medical care based on the injury, established by medical records contained in the claim file. Approved medical care or services would be consistent with the care and services normally approved under the appropriate state statute. Once the MSA projection report is received, the process is as follows: The final settlement documents should be sent to CMS by the MSA vendor. Once submitted, final approval by CMS could take anywhere from 3 to 6 months. Advise the injured worker or their counsel of the anticipated time for final settlement of the claim due to review by CMS. When CMS has approved the MSA (with or without modifications), the matter is ready for finalization. Final settlement paperwork should then be submitted to CMS. Confidential, Proprietary and Trade Secret Document of NARS and protected by the Florida Uniform Trade Secrets Act, chapter 688, Florida Statutes. No use allowed unless specifically authorized.
 Y(Our) Workers' Compensation Guidebook - The NARS Way Page 57 Page 59
Y(Our) Workers' Compensation Guidebook - The NARS Way Page 57 Page 59